More Information
Submitted: December 13, 2021 | Approved: May 05, 2022 | Published: May 06, 2022
How to cite this article: PérezPadrón-Arredondo G. Infection by SARS-CoV-2 in healthcare workers of a second level hospital. New Insights Obes Gene Beyond. 2022; 6: 012-016.
DOI: 10.29328/journal.niogb.1001018
Copyright License: © 2022 Padrón-Arredondo G. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; SARS-CoV-2; Healthcare workers; Nosocomial transmission; Asymptomatic carriers; Diagnostic testing
Infection by SARS-CoV-2 in healthcare workers of a second level hospital
Guillermo Padrón-Arredondo*
Research Department Hospital General Playa del Carmen, Av. Constituyentes s/n with Street 135 Col. Ejidal. Playa del Carmen, Quintana Roo. México CP: 77734
*Address for Correspondence: Guillermo Padrón-Arredondo, Research Department Hospital General Playa del Carmen, Av. Constituyentes s/n with Street 135 Col. Ejidal. Playa del Carmen, Quintana Roo. México CP: 77734, Email: [email protected]
Background: From the first COVID-19 case in Playa del Carmen, 370 cases of infection have been reported in our staff until December 31, 2020.
Material and methods: Study in workers of the General Hospital who developed SAR-CoV-2 infection during the pandemic. A sample of 30 cases of both sexes with laboratory-confirmed infection was obtained. Descriptive statistics were used with measures of central tendency, dispersion and percentages.
Results: In a sample of 30 workers there were 13 doctors, 6 nurses and 11 support workers. The age was obtained as a mean of 38.8 years and SD = 10.4. Only four risk factors were found. Of the 30 infected health workers, 27 were treated on an outpatient basis and three required hospitalization.
Discussion: The main symptoms in health workers are alterations in the sensation of taste and smell, but unlike our study, was headache, fever and myalgia. Likewise, it has been observed that medical are the most affected, but in this study it was support and the least affected was nursing personnel. There is no doubt that asymptomatic carriers are a serious disease transmission problem such that transmission between health workers by asymptomatic carriers is possible as was observed in this analysis.
From the beginning of the pandemic in Wuhan, China and its importation to Mexico on February 29, to the state of Quintana Roo on March 13, and the first case of infection was presented in the personnel working in our hospital on March 30, 2020. From the first case, there have been 236 cases of infection in our staff until December 31, 2020. There is a social perception that the acquisition of the COVID-19 disease is higher in the hospital environment in such a way that the community avoids going to hospitals to avoid contagion, however, community infection is more frequent and lethal [1].
The infection by the SARS-CoV-2 virus that causes the COVID-19 disease in the personnel working in hospitals is very important due to the lack of medical and nursing personnel and the shortage of hospital units in our country, which makes them indispensable for the health care of the general population, for which their absolute protection is of vital importance [2]. In our hospital, tests were performed only on personnel with symptoms suggestive of viral infection [3].
Observational, descriptive, prevalence and analytical study in working patients of the Playa del Carmen General Hospital who were diagnosed with SARS-CoV-2 infection during the pandemic. From April to December of the year 2020. For this, a sample of 30 health worker patients was recruited in our hospital of both sexes and from most of the hospital work shifts and from all work areas that presented infection by the SARS-CoV-2 laboratory-confirmed and randomly selected by the question did you get sick from COVID? And if so, they were asked for authorization to apply a survey designed by the author. Descriptive statistics were used with measures of central tendency and dispersion, as well as percentages.
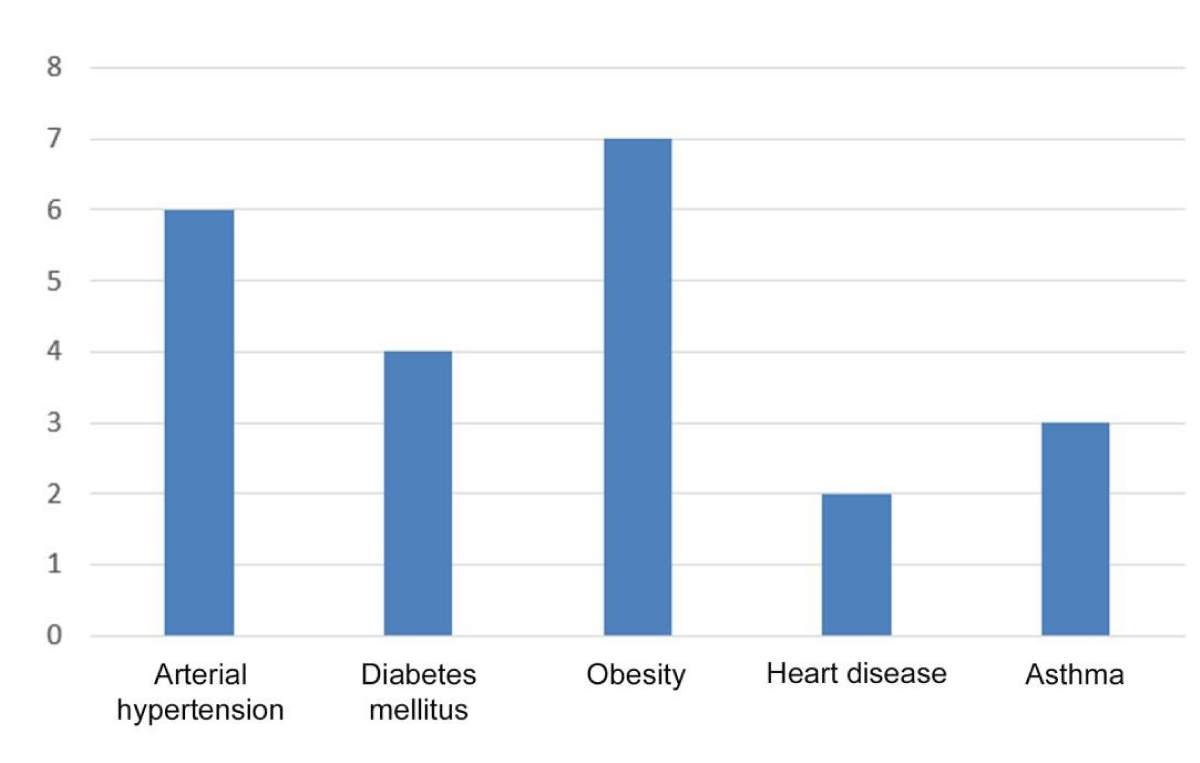
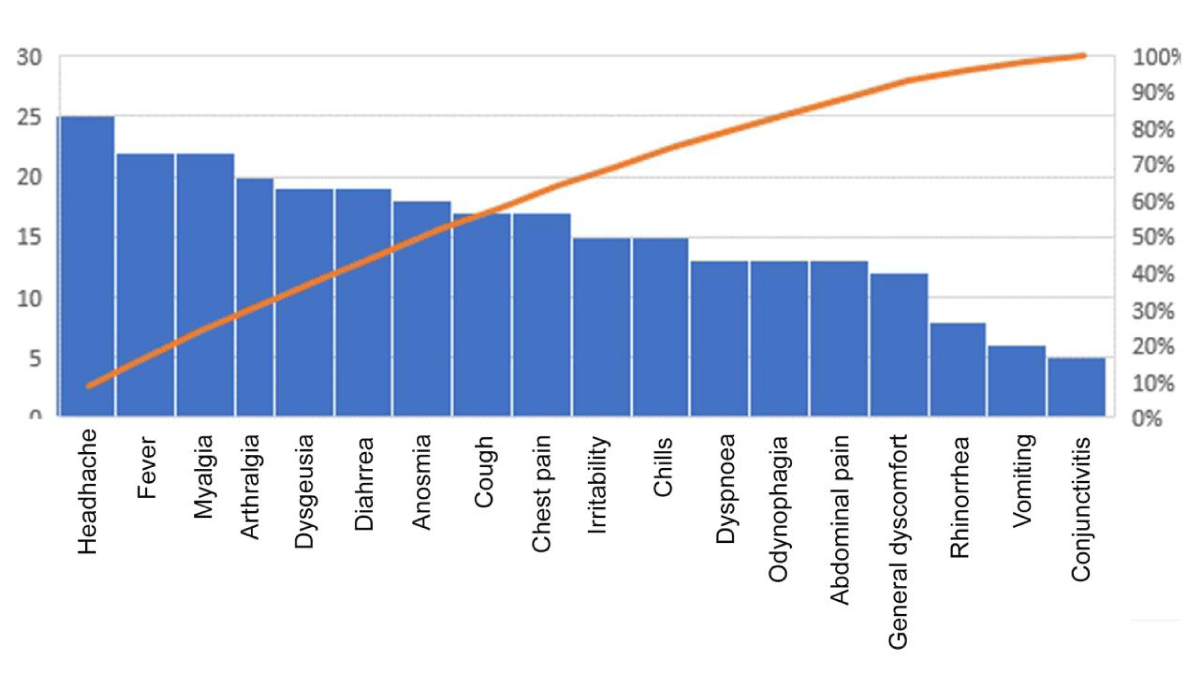
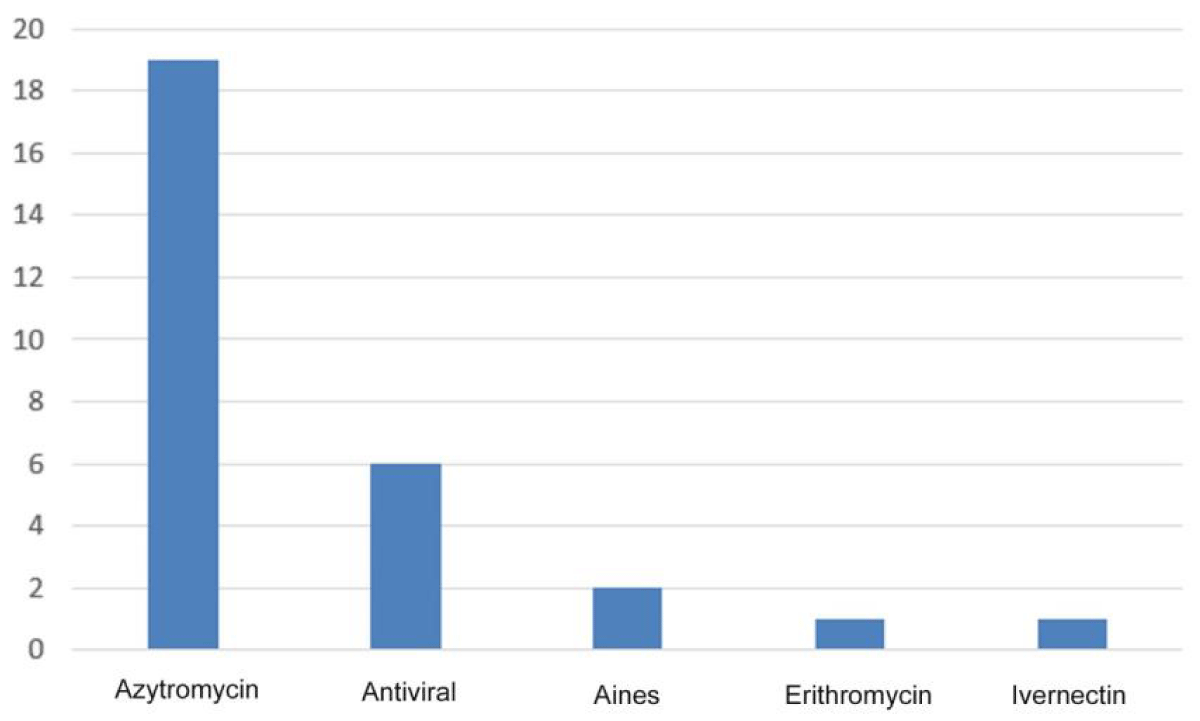
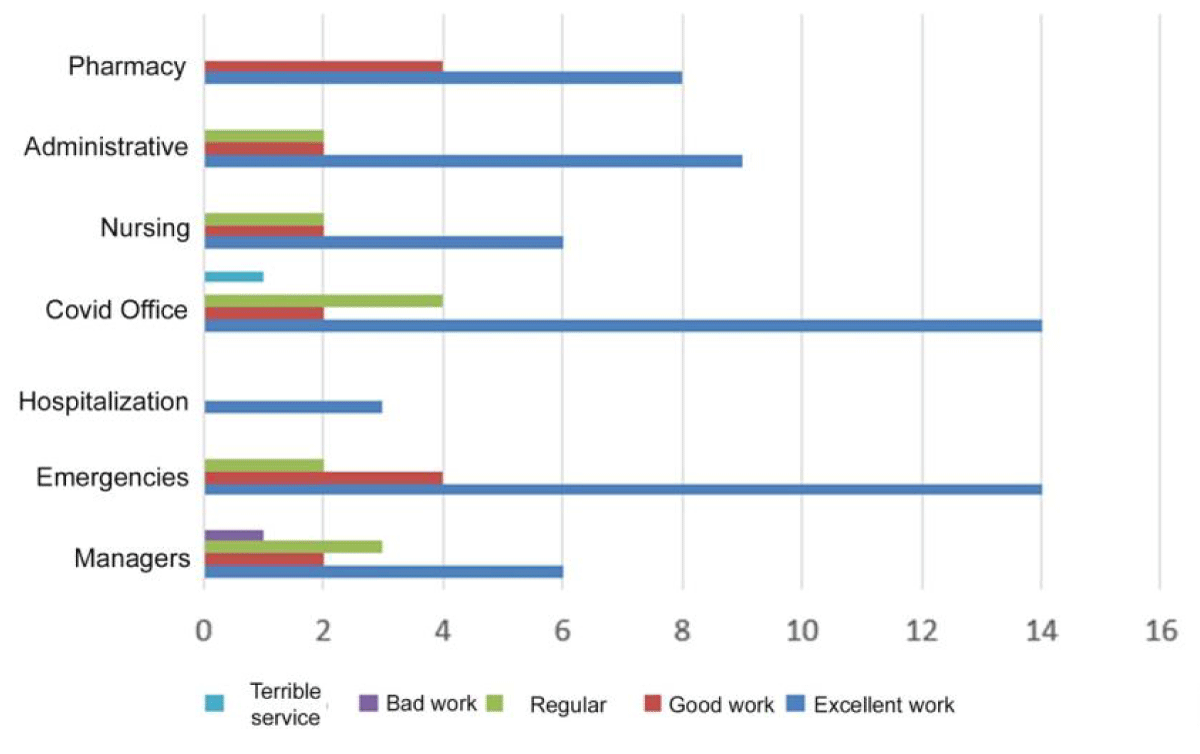
In a sample of 30 patients, there were 13 doctors, 6 nurses and 11 support personnel (quartermaster, administrative). The demographic data are presented in Table 1. Regarding work shifts, they were the following: Morning Shift = 7; Evening = 11, Evening A 1; Nocturnal B 5 and Special Daytime = 6. Total 30 (only the workers of the special Night shift were not surveyed). Regarding the age of the patients, a mean of 38.8 years was obtained with SD = 10.4, the youngest worker with 23 and the oldest with 59 and a range of 36 years. Only four risk factors were found in this study group (Figure 1). The clinical picture of the patients is presented in Figure 2, (only one patient had no symptoms, but was positive for SARS-CoV-2). Of the 30 health workers infected, 27 (90%) were treated on an outpatient basis, three cases (10%) required hospitalization. The treatment of patients is presented in Figure 3. Regarding the perception of treatment as patients by hospital staff, it is presented in Figure 4. About the perception of the health workers surveyed, they perceived the management of the pandemic in the hospital as follows: Excellent [13 (43%), Good 12 (40%) and Fair 1 (3%) and four 14%) had no opinion]; Finally, regarding the question of whether they would be vaccinated against SARS-CoV-2, 26 (87%) patients agreed and four disagreed (13%).
| Table 1: Demographic data of 30 healthcare workers infected with SARS-CoV-2. | ||
| Features | Health workers | % |
| Total | 30 | (100) |
| Sex | ||
| -Female | 15 | (50) |
| -Male | 15 | (50) |
| Total | 30 | (100) |
| Age (years) | ||
| 20 to 29 | 7 | (23) |
| 30 to 39 | 9 | (30) |
| 40 to 49 | 9 | (30) |
| 50 to 59 | 5 | (17) |
| Total | 30 | (100) |
| Ocupation | ||
| Doctors | 11 | (38) |
| - Undergraduate interns | 2 | |
| -Generals | 5 | |
| -Specialists | 3 | |
| -Dentists Nurses |
1 6 |
(18) |
| Support | 13 | (44) |
| -Cooks | 6 | |
| -Stretcher bearers | 2 | |
| -Administrative | 5 | |
| Total | 30 | (100) |
| Number of Symtoms | ||
| 0 | 1 | (3) |
| 3 | 1 | (3) |
| 4 | 1 | (3) |
| 6 | 4 | (13) |
| 7 | 3 | (10) |
| 9 | 5 | (18) |
| 10 | 4 | (13) |
| 11 | 2 | (7) |
| 12 | 3 | (10) |
| 13 | 3 | (10) |
| 15 | 3 | (10) |
| Total | 30 | (100) |
Figure 1: Risk factors in 22 out of 30 healthcare workers infected with SARS-CoV-2.
Figure 2: Clinical picture in 29 of 30 health workers infected by SARS-CoV-2.
Figure 3: Treatment of 29 health workers from 30 cases infected by SARS-CoV-2. *One asymptomatic infected case did not receive any treatment.
Figure 4: Perception of treatment as patients by hospital staff in 30 patients infected by SARS-CoV-2.
In the work of Lombardi, et al. [4], they found that the main symptoms in health workers were alterations in the sensation of taste and smell, unlike our study where they were found as the main symptoms in suspects of COVID-19 headache, fever, and myalgia in that order. Likewise, in this study, the medical staff was the most affected, unlike what was found in our study, which was the support staff, and the least affected was the nursing staff.
Gómez-Ochoa, et al. [5] in their large study found that the nursing staff (48%) presented the majority of cases, unlike what was found in our study (18%); likewise, the prevalent symptoms were anosmia, fever and myalgia, while we had fever, headache and myalgia. They found 5% severe disease and 0.5% mortality. Unlike us where there were only two severe cases [7% (without intubation)] and no deaths.
Woo Jeon Y, et al. [6] in their study found that healthy carriers are a major public health problem because of 30 asymptomatic patients who came to the hospital and were subsequently diagnosed as positive for COVID-19, they had contact with 184 workers from The health of the hospital who underwent a diagnosis by RT-PCR 126 workers at the beginning of the contact, at 14 days and a month after exposure, all being free of infection at the end of the follow-up previously classified into four risk groups.
In the work of Lombardi, et al. [4], they found that the main symptoms in health workers were alterations in the sensation of taste and smell, unlike our study where they were found as the main symptoms in suspects of COVID-19 headache, fever, and myalgia in that order. Likewise, in this study, the medical staff was the most affected, unlike what was found in our study, which was the support staff, and the least affected was the nursing staff.
Gómez-Ochoa, et al. [5] in their large study found that the nursing staff (48%) presented the majority of cases, unlike what was found in our study (18%); likewise, the prevalent symptoms were anosmia, fever and myalgia, while we had fever, headache and myalgia. They found 5% severe disease and 0.5% mortality. Unlike us where there were only two severe cases [7% (without intubation)] and no deaths.
Woo Jeon Y, et al. [6] in their study found that healthy carriers are a major public health problem because of 30 asymptomatic patients who came to the hospital and were subsequently diagnosed as positive for COVID-19, they had contact with 184 workers from The health of the hospital who underwent a diagnosis by RT-PCR 126 workers at the beginning of the contact, at 14 days and a month after exposure, all being free of infection at the end of the follow-up previously classified into four risk groups.
Petrakis, et al. [7] report that SARS CoV-2 infection presents a higher risk of complications in elderly people and those with cardiopulmonary diseases, but recent research affirms that obesity is a major risk factor for serious complications, same observation that is presented in our study because this risk factor was present more frequently. This is due to the peroxidation of lipids that lipid aldehyde creates, which in the COVID-19 scenario affect its prognosis.
Erener S [8] in his review refers that multiple studies have shown that Diabetes mellitus is a risk factor for all types of bacterial, viral and fungal infections, in such a way that in the context of SARS-CoV-2 infection it is has shown that this risk factor increases both morbidity and mortality in COVID-19 patients. Bello-Chavolla, et al. [9] have developed a clinical score to identify the risk of complications in these patients that may be useful in primary health care.
Pugliese, et al. [10] remind us that Diabetes mellitus by itself is not a risk factor for acquiring SARS-CoV-2 infection but it is for the risk of serious complications in the event of acquiring the disease together with other comorbidities typical of adulthood.
Kumar Singh, et al. [11] also analyzed hypertension as a risk factor associated with other diseases and recommend that in those patients under antihypertensive treatment with inhibitors of the renin-angiotensin system [ACE -2 (enzyme angiotensin converting) and ARB, angiotensin receptor blockers)] continue due to their importance in these patients.
Johnston [12] recognizes asthma as a risk factor mainly in older smokers and also the usefulness of macrolides as adjuvants in the treatment of COVID-19, which is confirmed in our study since most of our cases received Azithromycin. García-Moguel, et al. [13] treated two patients with asthma associated with COVID-19 with positive results, recommending that their own asthma treatment should not be discontinued in these settings because it seems that this treatment helps the management of the viral infection. In our sample we also had two cases associated with asthma, conventional treatment and adequate recovery.
Lan, et al. [14] in their analysis found that monitoring of temperature and symptoms in all individuals is very important and found that anosmia, ageusia, fever, and myalgia are the important independent predictors in positive analyzes. A little different from what was found in this study, although they emphasize that symptoms associated with nasal congestion and sore throat were associated with negative cases for infection.
Tests for the diagnosis of COVID-19 in the general population are less than impossible to perform, but for health worker personnel it is possible and in a study by Clemency, et al. [15] they found that, in a group of workers with at least three clinical data such as fever, loss of taste and smell could discriminate patients with COVID-19 and thus reduce the transmission of the disease in the personnel of health and their families. In our study, only the workers who presented any symptoms of the 18 analyzed were subjected to the test and all were positive.
Onoda, et al. [16] remind us that the types of tests available for the diagnosis of this disease are: Nucleic acid detection tests (polymerase chain reaction or PCR). 2. Antigen detection tests. 3. Antibody detection tests (IgG, IgM). In this study, all workers underwent PCR and in one case the PCR plus the antibody detection test.
The role of imaging in this infection has been extensively analyzed and Castillo, et al. [17] make an extensive review of the subject. In our patients, none mentioned having undergone any of these studies, perhaps due to their outpatient management and the mild to moderate severity of the clinical picture.
Chaccour, et al. [18] present a study on the pharmacological treatment of COVID-19 with ivermectin, a drug that was ultimately not approved by the WHO.
In our patients, these were treated with paracetamol in all cases, antibiotic (azithromycin) in most cases, one case with erythromycin and in another case ivermectin was used. One patient was personally treated with azithromycin, moxifloxacin, prednisone, methylprednisolone, and tocilizumab).
There is no doubt that healthy carriers are a serious disease transmission problem and Lai, et al. [19] emphasize the importance of the issue because the disease is.
It can present, in addition to an asymptomatic carrier, as an acute respiratory disease and finally as severe pneumonia, in such a way that transmission between workers of health by asymptomatic carriers is possible as observed in this analysis.
Finally, it has been shown by Jones, et al. [20] that infection prevention and health personnel control measures (control tests) are effective for the control of the pandemic in both asymptomatic and symptomatic workers and their families mainly Those who work in the areas with the highest risk of direct contagion, such as COVID clinics and the respiratory care hospitalization area where patients with moderate and severe disease are concentrated, where only in this group studied we had two cases that recovered satisfactorily.
- Zheng C, Hafezi-Bakhtiari N, Cooper V, Davidson H, Habibi M, Riley P, Breathnach A. Characteristics and transmission dynamics of COVID-19 in healthcare workers at a London teaching hospital. J Hosp Infect. 2020 Oct;106(2):325-329. doi: 10.1016/j.jhin.2020.07.025. Epub 2020 Jul 28. PMID: 32730771; PMCID: PMC7384992.
- Barranco R, Ventura F. Covid-19 and infection in health-care workers: An emerging problem. Med Leg J. 2020 Jul;88(2):65-66. doi: 10.1177/0025817220923694. Epub 2020 May 22. PMID: 32441196.
- Rivett L, Sridhar S, Sparkes D, Routledge M, Jones NK, Forrest S, Young J, Pereira-Dias J, Hamilton WL, Ferris M, Torok ME, Meredith L; CITIID-NIHR COVID-19 BioResource Collaboration, Curran MD, Fuller S, Chaudhry A, Shaw A, Samworth RJ, Bradley JR, Dougan G, Smith KG, Lehner PJ, Matheson NJ, Wright G, Goodfellow IG, Baker S, Weekes MP. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020 May 11;9:e58728. doi: 10.7554/eLife.58728. PMID: 32392129; PMCID: PMC7314537.
- Lombardi A, Consonni D, Carugno M, Bozzi G, Mangioni D, Muscatello A, Castelli V, Palomba E, Cantù AP, Ceriotti F, Tiso B, Pesatori AC, Riboldi L, Bandera A, Lunghi G, Gori A. Characteristics of 1573 healthcare workers who underwent nasopharyngeal swab testing for SARS-CoV-2 in Milan, Lombardy, Italy. Clin Microbiol Infect. 2020 Oct;26(10):1413.e9-1413.e13. doi: 10.1016/j.cmi.2020.06.013. Epub 2020 Jun 20. PMID: 32569835; PMCID: PMC7305713.
- Gómez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Díaz ZM, Wyssmann BM, Guevara SLR, Echeverría LE, Glisic M, Muka T. COVID-19 in Health-Care Workers: A Living Systematic Review and Meta-Analysis of Prevalence, Risk Factors, Clinical Characteristics, and Outcomes. Am J Epidemiol. 2021 Jan 4;190(1):161-175. doi: 10.1093/aje/kwaa191. Erratum in: Am J Epidemiol. 2021 Jan 4;190(1):187. PMID: 32870978; PMCID: PMC7499478.
- Woo Jeon Y, Suk Park E, Jae Jung S, Kim Y, Yong Choi J, Hang Kim H. Protection of Healthcare Workers Against COVID-19 at a Large Teaching Hospital in Seoul, Korea, Yonsei Med J. 2020; Jul; 61(7):631-4. https://doi.org/10.3349/ymj.2020.61.7.63
- Petrakis D, Margină D, Tsarouhas K, Tekos F, Stan M, Nikitovic D, Kouretas D, Spandidos DA, Tsatsakis A. Obesity ‑ a risk factor for increased COVID‑19 prevalence, severity and lethality (Review). Mol Med Rep. 2020 Jul;22(1):9-19. doi: 10.3892/mmr.2020.11127. Epub 2020 May 5. PMID: 32377709; PMCID: PMC7248467.
- Erener S. Diabetes, infection risk and COVID-19. Mol Metab. 2020 Sep;39:101044. doi: 10.1016/j.molmet.2020.101044. Epub 2020 Jun 23. PMID: 32585364; PMCID: PMC7308743.
- Bello-Chavolla OY, Bahena-López JP, Antonio-Villa NE, Vargas-Vázquez A, González-Díaz A, Márquez-Salinas A, Fermín-Martínez CA, Naveja JJ, Aguilar-Salinas CA. Predicting Mortality Due to SARS-CoV-2: A Mechanistic Score Relating Obesity and Diabetes to COVID-19 Outcomes in Mexico. J Clin Endocrinol Metab. 2020 Aug 1;105(8):dgaa346. doi: 10.1210/clinem/dgaa346. PMID: 32474598; PMCID: PMC7313944.
- Pugliese G, Vitale M, Resi V, Orsi E. Is diabetes mellitus a risk factor for COronaVIrus Disease 19 (COVID-19)? Acta Diabetol. 2020 Nov;57(11):1275-1285. doi: 10.1007/s00592-020-01586-6. Epub 2020 Aug 31. PMID: 32865671; PMCID: PMC7456750.
- Singh AK, Gupta R, Misra A. Comorbidities in COVID-19: Outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr. 2020 Jul-Aug;14(4):283-287. doi: 10.1016/j.dsx.2020.03.016. Epub 2020 Apr 9. PMID: 32283499; PMCID: PMC7144598.
- Johnston SL. Asthma and COVID-19: Is asthma a risk factor for severe outcomes? Allergy. 2020 Jul;75(7):1543-1545. doi: 10.1111/all.14348. PMID: 32358994; PMCID: PMC7267381.
- García-Moguel I, Díaz Campos R, Alonso Charterina S, Fernández Rodríguez C, Fernández Crespo J. COVID-19, severe asthma, and biologics. Ann Allergy Asthma Immunol. 2020 Sep;125(3):357-359.e1. doi: 10.1016/j.anai.2020.06.012. Epub 2020 Jun 14. PMID: 32553608; PMCID: PMC7293849.
- Lan FY, Filler R, Mathew S, Buley J, Iliaki E, Bruno-Murtha LA, Osgood R, Christophi CA, Fernandez-Montero A, Kales SN. COVID-19 symptoms predictive of healthcare workers' SARS-CoV-2 PCR results. PLoS One. 2020 Jun 26;15(6):e0235460. doi: 10.1371/journal.pone.0235460. PMID: 32589687; PMCID: PMC7319316.
- Clemency BM, Varughese R, Scheafer DK, Ludwig B, Welch JV, McCormack RF, Ma C, Nan N, Giambra T, Raab T. Symptom Criteria for COVID-19 Testing of Heath Care Workers. Acad Emerg Med. 2020 Jun;27(6):469-474. doi: 10.1111/acem.14009. Epub 2020 Jun 8. PMID: 32396670; PMCID: PMC7272901.
- Onoda M, Martínez Chamorro MJ. Pruebas diagnósticas de laboratorio de COVID-19. Grupo de Patología Infecciosa de la Asociación Española de Pediatría de Atención Primaria. Abril de 2020. Disponible en: [https://aepap.org/grupos/grupo-de-Patologiainfecciosa/contenido/documentos-delgpi]
- Castillo AF, Bazaes ND, Huete GÁ. Radiología en la Pandemia COVID-19: Uso actual, recomendaciones para la estructuración del informe radiológico y experiencia de nuestro departamento, Rev Chil Radiol. 2020; 26(3): 88-99.
- Chaccour C, Ruiz-Castillo P, Richardson MA, Moncunill G, Casellas A, Carmona-Torre F, Giráldez M, Mota JS, Yuste JR, Azanza JR, Fernández M, Reina G, Dobaño C, Brew J, Sadaba B, Hammann F, Rabinovich R. The SARS-CoV-2 Ivermectin Navarra-ISGlobal Trial (SAINT) to Evaluate the Potential of Ivermectin to Reduce COVID-19 Transmission in low risk, non-severe COVID-19 patients in the first 48 hours after symptoms onset: A structured summary of a study protocol for a randomized control pilot trial. Trials. 2020 Jun 8;21(1):498. doi: 10.1186/s13063-020-04421-z. PMID: 32513289; PMCID: PMC7276958.
- Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, Ko WC, Hsueh PR. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J Microbiol Immunol Infect. 2020 Jun;53(3):404-412. doi: 10.1016/j.jmii.2020.02.012. Epub 2020 Mar 4. PMID: 32173241; PMCID: PMC7128959.
- Jones NK, Rivett L, Sparkes D, Forrest S, Sridhar S, Young J, Pereira-Dias J, Cormie C, Gill H, Reynolds N, Wantoch M, Routledge M, Warne B, Levy J, Córdova Jiménez WD, Samad FNB, McNicholas C, Ferris M, Gray J, Gill M; CITIID-NIHR COVID-19 BioResource Collaboration, Curran MD, Fuller S, Chaudhry A, Shaw A, Bradley JR, Hannon GJ, Goodfellow IG, Dougan G, Smith KG, Lehner PJ, Wright G, Matheson NJ, Baker S, Weekes MP. Effective control of SARS-CoV-2 transmission between healthcare workers during a period of diminished community prevalence of COVID-19. Elife. 2020 Jun 19;9:e59391. doi: 10.7554/eLife.59391. PMID: 32558644; PMCID: PMC7326489.